Trauma Specific Psychotherapy
1) Introduction / Definitions
Trauma has long been a major focus for the majority of schools of Psychotherapy. Consequently, a deep empirical understanding of the traumatic symptoms and effects as well as treatments have long been established.
A renewed focus on Trauma ('3rd wave') started to shape scientific research starting as early as the 80s and 90s and gathering even more momentum since 2000, significantly aided through the contribution of Neuroscience and Neurobiology [B. van der Kolk, Hartmann, Perry, O. van der Hart, Nijenhuis, Steele, Baldwin, Ogden, Levine, Siegel, Porges, Lanius, Parnell, Schwartz, et al.].
A 'traumatic experience' (see below) can lead to Psychological Trauma:
Psychological Trauma can be defined as: a type of damage to the mind and nervous system that occurs as a result of a severely distressing event, series of events or with ongoing situations that causes stress that is overwhelming and unbearable in its nature and /or changes the perception of the world and / or the self in a dramatic way and can't be integrated / resolved.
Typically, a sufferer would experience intense fear, panic, anger, confusion, loss of consciousness, power- and helplessness to avert, protect or change a situation. This helplessness is of clinical significance.
After the traumatic experience a person might suffer from Post-traumatic Stress (PTS) with significant symptoms. These symptoms are partially due to the imbalance of the two branches of the Autonomous Nervous System (ANS): the Sympathetic and the Parasympathetic Nervous System.
Extreme Post-traumatic stress when (medically) diagnosed, is called Post-traumatic Stress Disorder or PTSD.
As diagnosis is commonly based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) and follows a Psychiatric or Medical Model, which is not the concern of this article and website, the term PTSD will be used here in the more generic form.
Not everyone who was exposed to a traumatic experience develops PTSD which is an outcome of a complex interaction between trauma intensity, personal vulnerability and resources.
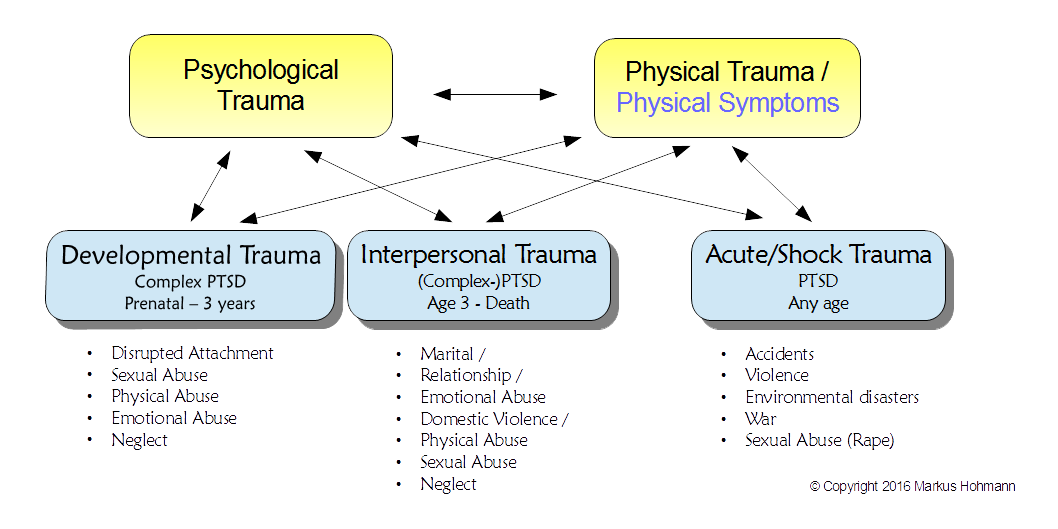
There are three categories of Psychological Trauma or PTSD: Developmental, Interpersonal and Shock Trauma:
- Developmental Trauma (DT) , a more recent category, is also called Complex Trauma or Complex PTSD (C-PTSD) captures the earliest traumatic experiences from pre-natal to about 3 years of age. This can consist of a combination of: neglect, disrupted attachment (see: Attachment Theory), emotional, physical or sexual abuse. This is typically the first level in what often is a cumulative experience for sufferers. Although it is wide spread it still needs a lot more research. The younger the person - and here we are talking about pre-natal age to 3 years of age - the more difficult it is to research.
- Interpersonal Trauma (IPT) describes trauma experiences which occur after 3 years of age. It is part of Complex Trauma when these experiences occurred in childhood. These traumatic experiences usually continued over a prolonged period of time and might consist of neglect and / or a variety of abuse (see diagram) but typically does not include the disrupted attachment of infancy. However, as described further down, IPT might continue from and build on DT.
- Acute / Shock Trauma (ST) can be caused by accidents, violence, environmental disasters, war, sexual abuse / rape. This category was the main focus of PTSD-research for a long time and is the most researched and understood in the trauma field.
2) The Effect of Trauma On The Nervous System
The normal physiological response to severe stress / danger is either hyper-arousal and a readiness for fight and flight (Sympathetic Nervous System) or when this is unsuccessful, hypo-arousal with a freeze response – a protective response for survival.
While this was known for a long time, the birth of three new disciplines led to a vast acceleration of knowledge about the effects of Psychological Trauma: Neuroscience, Developmental Psychopathology and Interpersonal Neurobiology.
“Research from these new disciplines has revealed that trauma produces actual physiological changes, including a recalibration of the brain's alarm system, an increase in stress hormone activity, and alterations in the system that filters relevant information from irrelevant. We now know that trauma compromises the brain area that communicates the physical, embodied feeling of being alive. These changes explain why traumatized individuals become hyper[- or hypo-]vigilant to threat at the expense of spontaneous engaging in their day-to-day lives” [Bessel van der Kolk: The Body Keeps The Score, 2014]
Sensory information (sight, smell,sound, kinesthetic, etc.) arrive in a part of the limbic system called the Thalamus which is the first step of processing. From there the information is passed on in two direction: to the Amygdala (in the unconscious part of the brain) and the frontal lobes where it reaches conscious awareness.
The main function of the Amygdala (“the brain's smoke detector”) is to identify if the information is relevant for our survival [Kolk, LeDoux, Feinstein]. If the Amygdala, with the help of the Hippocampus, detects a threat it sends an instant message to the Hypothalamus and brain stem, releasing powerful stress hormones and activating the Sympathetic Nervous System (SNS).
Following a traumatic experience this system may stay activated permanently and causes the increased misinterpretation of risk.
People with PTSD suffer the consequences of a functional (and subsequent structural) neurological change that occurred following the traumatic experience. They suffer from almost constant hyper- or hypo-arousal even decades later. The feelings and sensations involved overwhelm the nervous system: taking all the resources of the person (to cope) and at times can leave little for conscious awareness, memory, decision making and spontaneous engagement, etc. Something most people take for granted. Further, they may suffer from a variety of physical symptoms and conditions (see below).
People with PTSD “try to shut themselves down and develop tunnel vision and hyperfocus. If they can't shut down naturally, they may enlist drugs or alcohol to block out the world. The tragedy is that the price of closing down includes filtering out sources of pleasure” [Van Der Kolk].
Porges suggested the Polyvagal Theory to explain how people deal with trauma. This theory might further explain the wide variety of physical symptoms and conditions that are observed. There are several branches of the vagal nerve reaching the inner organs (stomach, digestive tract, lungs, heart, spleen, liver, kidneys, etc.). They are working via the Parasympathetic Nervous System (PNS).
The vagus system is in opposition to sympathetic-adrenal system, which is involved in mobilization and the fight-and-flight response. The 'vagal tone' represents the amount of vagal activity in an organism and therefore the balance of the ANS and can be used as a physiological marker for vulnerability to stress (also see: Respiratory Sinus Arrhythmia (RSA) and Heart Rate Variability (HRV) .) The vagus nerve plays a major part in the inflammatory reflex which controls the innate immune responses and inflammation.
3) Trauma Related Symptoms
Depending on the type and severity of the trauma and the individual's personal and social resources there is broad spectrum of symptoms that can be observed. This, originally made it difficult to research and understand trauma. The aforementioned symptoms stretch from physical to emotional, behavioural, cognition, concept of self and dissociation.
“Dissociation is the essence of trauma. The overwhelming experience is split off and fragmented, so that the emotions, sounds, images, thoughts, and physical sensations related to the trauma take on a life of their own. The sensory fragments of memory intrude into the present, where they are literally relived.” [Van Der Kolk]
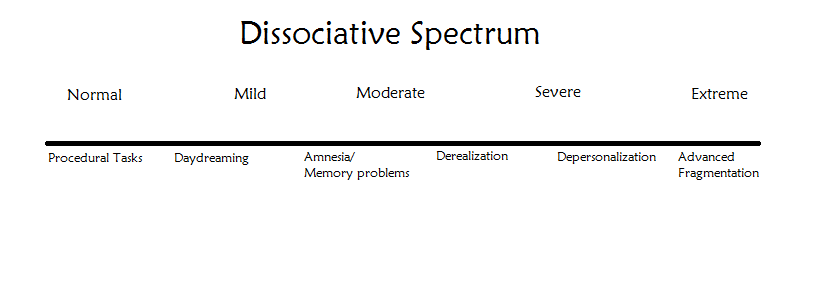
In practice we can observe a broad spectrum of dissociation:
Many people would have any number of symptoms on the scale but depending how much of each might determine where they might identify themselves to be on the scale.
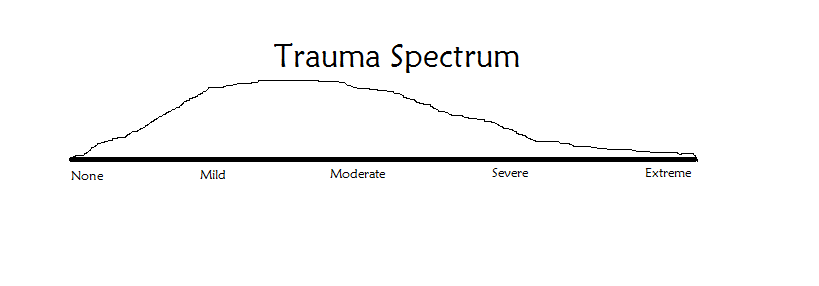
A typical representation (spread) in the population might be:
This graph suggests that dissociation and trauma is wide spread in the population, especially when Developmental Trauma is taken into consideration (see below).
But lets return to the symptoms that affect the body and mind in general:
As quoted above, the fragmented parts that are showing up in daily life can cause difficulties with:
1. Affect (emotional self-) regulation:
decreased regulation of stress and defensive states, ability to maintain or increase positive feelings, identifying emotions and internal states, compulsive or extremely inhibited sexuality
2. Behavioural control:
impulse control, aggression, compulsive self-soothing
3. Cognition:
attention, concentration, confusion, planning, judgement, initiation, self-monitoring, processing new information, completing tasks, object constancy, 'cause-effect' thinking, language and communication abilities
4. Dissociation:
amnesia / memory loss, derealization, depersonalization, altered states of consciousness and fragmentation (of personality)
5. Emotions / Psychological states:
agitation, shock, anger, irritability, mood swings, fear and anxiety, guilt, shame, self-blame, self-isolation, sadness, grief, hopelessness, despair, depression, feeling disconnected or numb, eating disorders, personality disorders, suicidality, paradoxical gratitude for or idealization of a perpetrator,
6. Physical wellbeing:
Insomnia, nightmares, fatigue, startle effect, increased heart rate, aches and pains, muscle tension, auto-immune conditions, irritable bowel syndrome, obesity, certain types of asthma, diabetes, heart disease and stroke, further: alcohol-, drug- and smoking related conditions and illnesses, injuries and self inflicted injuries,etc. as well as reduced life expectancy.
[adapted from: Cook, Blaustein, Spinazzola, Van Der Kolk, 2003 & 2005]
4. Childhood Trauma - A Hidden Epidemic
In the mid-80s Vincent Felitti was chief of Kaiser Permanente's Department of Preventative medicine in San Diego, California, which was the largest medical screening program in the world at the time.
These screening results, in conjunction with Centres for Disease Control and Prevention, led to the Adverse Childhood Experiences (ACE) Study in 1995 and 1997, a mass scale, longitudinal study.
The 17337 participants were volunteers who were interviewed about 10 types of childhood trauma: physical abuse, sexual abuse, emotional abuse, physical neglect, emotional neglect, mother treated violently, household substance abuse, household mental illness, parental separation and divorce, incarcerated household member.
“The ACE study revealed that traumatic life experiences during childhood and adolescence are far more common then expected. The study respondents were mostly white, middle class, middle aged, well educated,and financially secure enough to have good medical insurance and yet only 1/3 of the respondents reported no adverse childhood experiences.” [Van Der Kolk]
The study found that ACEs were common: 28% reported physical abuse, 21% sexual abuse, many others reporting one of the other criteria. 40% reported two or more ACEs and 12.5% four or more.
The number of ACEs was strongly correlating with adulthood high-risk behaviours such as smoking, alcohol and drug abuse, promiscuity, severe obesity and ill-healths such as depression, heart disease, cancer, chronic lung disease and shortened life-span [Anda, Felitti, et al., 1998, 2003, Middlebrooks, Audage, 2008].
“The ACE study's results suggest that maltreatment and household dysfunction in childhood contribute to health problems decades later. These include chronic diseases—such as heart disease, cancer, stroke, and diabetes—that are the most common causes of death and disability in the United States (…) might reasonably be assumed to reflect similar trends in other parts of the world. ” [WHO, International Society for Prevention of Child Abuse and Neglect, 2006]
Since the ACE study many more have confirmed similar correlations between adverse childhood experience and symptoms in childhood, adolescence and adulthood.
This led to the creation of the new terms: 'Developmental Trauma' and 'Complex Trauma' .
At this point we need to add two more categories to the above list of trauma related symptoms:
7) Attachment
feeling vulnerable, insecure, hostile, avoidant, evasive, overly critical, lack of trust, social isolation, relationship boundaries, pervasive helplessness, paralysis of initiative
8) Biology
sensory-motor developmental dysfunctions, sensory-integration difficulties, somatization, and increased medical problems.
With such a wide extend of symptoms and spread in the population we can agree with Van Der Kolk when he calls it: “The Hidden Epidemic”.
5. Cumulative Effects Of Trauma
Sadly, following on from the ACE study and related studies, it was found that victims of abuse had an increased likelihood of re-victimization:
- Wyatt, Guthrie, and Notgrass (1992) found that 56% of abuse survivors compared with 21% of non-sexually abused women experienced adult sexual assault.
- Briere and Runtz (1987) found 49% of abused women compare to 18% non-abused women reported being battered by a partner
- Russell (1984) interviewing victims disclosing rape or attempted rape, found that more then 50% indicated prior sexual assault
- The “ACE study had shown that women who had an early history of abuse and neglect were seven times more likely to be raped in adulthood. Women who, as children, had witnessed their mothers being assaulted by their partners had a vastly increased chance to fall victim to domestic violence.” [ Felitti, 1998, cited in Van Der Kolk,2014]
There are numerous studies like these confirming the increased risk of re-traumatization.
Naturally, with the re-traumatization comes an increase in symptoms and severity of symptoms [see: Suliman, et al. 2009, and Follette, Polusny, Bechtle, Naugle, 1996, and Grasso, Green, Ford, 2013].
Some studies even suggest a trans-generational and cumulative effect from generation to generation.
Most of these studies are concerning people with severe and extreme levels of abuse and symptoms. However, as stated above, trauma is a spectrum of severity. It is likely that even with lower levels of trauma there is an increased risk of re-traumatization and therefore a cumulative effect for many trauma sufferers.
6. Treatments: Top-Down And Bottom-Up
Having looked at the spectrum, types and intensities of trauma, with an array of symptoms, all relating to a unique individual with a spectrum of internal and external supports and resources, there is one further variable to add: the trauma phase or stage.
Depending on these variables the treatment can rarely be as simple as a generic course of Cognitive Behavioural Therapy (CBT), though for some people with certain conditions and circumstances this works quite well.
There is a need to adapt the therapeutic treatments and interventions not only to the individual's experience and personality but to which phase s/he is in following the traumatic incident(s). A sensitive emotional attunement and following the cues of the client is still the best guide to what the client needs from treatment, aided by informed clinical discernment.
Principally, the need has been identified for a combination of two different therapeutic approaches (although in certain cases a temporary pharmacological intervention is warranted):
- Top-down: Psycho-education, Mindfulness and Mindfulness Based Stress Reduction (MBSR), CBT and Dialectical Behavioural Therapy (DBT) as well as Psycho-dynamic Psychotherapy (e.g. Humanistic and Integrative), all can be very helpful to the trauma sufferer to learn to deal with, understand, and integrate the traumatic experiences and symptoms.
- Bottom-up: Body Psychotherapy (e.g. Biodynamic- and Sensorimotor-), Somatic Experiencing, Eye Movement Desensitization and Re-integration (EMDR) all helping the somatic processing and resourcing of the client, also beneficial: Movement Therapy, Restorative Yoga, Massage and physical activities (sports), etc.
Finally, let's look at the proposed therapeutic approach regarding the different stages of Trauma Recovery [adapted from: Herman (1992); Van Der Kolk, Van Der Hart, Burbridge (1995); Van Der Kolk, et al. (2005); Ogden (2006); Fisher (2008)].
During all stages the goal is to achieve a safe and stable living in the here-and-now which allows the client to safely remember the trauma, rather then continue to re-live it.
Stage Ⅰ: Safety And Stabilization: Overcoming Dysregulation
- Already as part of building a connection, a safe and warm relationship and building trust, and in the presence of symptoms or the reporting of trauma-related experiences, the therapist should start to teach the client about the effects of trauma: to recognize symptoms, understand the meaning of overwhelming body sensations, intrusive emotions, and distorted cognitive schemas. Naturally, this has to be done in the most sensitive manner.
- Re-establishing bodily safety : working towards abstinence from high-risk and harmful behaviour, e.g. self-injury, persistent alcohol and drug use.
- Re-establishing a safe environment : working towards a secure living situation, non-abusive relationships, regular income, adequate supports.
- Re-establishing emotional stability : developing skills and somatic resources for stabilization and Self-Regulation: self-sooth, manage post-traumatic symptoms triggered by mundane events, ability to tolerate trauma-related physical sensations and emotions, regulate impulses, breathing for balancing the nervous system, developing a somatic sense of boundary.
- Fostering Resilience: health and self-care, composure, acceptance, perspective, collaboration and support through social engagement, tenacity, vision and hope.
Stage Ⅱ: Processing Traumatic Memories
- The experience of a secure attachment, as fostered within the therapeutic relationship, is important in regulating emotional arousal at this stage.
- The identification of feelings by verbalizing (and metabolising) somatic states, supported by the Psychotherapist.
- Deconditioning of traumatic memories and responses by controlled and safe activation.
- The correction of faulty traumatic beliefs which cause the associated shame.
- Using Interoception and Mindfulness when working at the edge of the window of tolerance (states of Hyper- and Hypoarousal).
- Learning 'Acts of Triumph': overcoming one's sense of helplessness.
Stage Ⅲ: Integration And Rehabilitation: A New Sense Of Self
- Restructuring of trauma-related schemes of internal and external reality (perception of self and the world, self-efficacy, capacity for trust and intimacy, communicating needs, empathy for others) through self-reflective processing.
- Exposure to restitutive experiences: feelings of mastery and pleasure, physical activities, sports and wilderness ventures, gratifying physical experiences
- Relational engagement
- Positive affect enhancement
In practice these stages are not time-linear or sequential. The first stage can take a long time and sadly, some people might not progress beyond this stage.
Even when the second and third stage has started, the first one will need to be revisited regularly to strengthen safety, stabilization and skills, depending on the individual client.
7) Synthesis And Application
I have worked with this model for some time now and find it to be most useful and often even surprisingly effective. Clients who have had years of severe suffering had started to turn this around within a few months. They are now on a path of recovery.
Some clients were initially not aware of being affected by a traumatic experience, some due to protective/defensive structures (denial), because it wasn't rape or penetration, others did not access the memory, etc.; but they did realize eventually the effect and symptoms that certain experiences had on them: guilt, shame, self-hatred, self-sabotage, fear, years of being shut-down, anger and rage, drug use and many more..
This model has been synthesized from research presented above and many teachers in the field of Psychotherapy as well my own experience working with many clients.
A model is a model, but in the end, outcomes are influenced and achieved by the person to person contact in the present moment. Further research will bring more clarity about treatment but the application always needs the fine tuning in the therapeutic relationship in any given moment.
In this sense, I am looking forward to continuing to apply and to learn.
© Copyright 2016-2024, Markus Hohmann